For some of you, these symptoms are keeping you from enjoying life with family, friends, work, and hobbies.
Knowledge is power when it comes to your health. This page sheds light on the conditions causing your symptoms, how they may be inter-related, and your best options for treatment. At VSS our goal is to listen to your concerns and address them in a way that improves your quality of life.
There are two primary veins in your abdomen and pelvis where compression occurs and several secondary sites. The primary sites are the deep veins that drain the pelvis and the legs (iliac vein) and the vein that drains the left kidney (renal vein).
The symptoms and clinical picture vary by the vein affected. By understanding how these conditions are different, yet at times interrelated, can help you make a better health care decision.

Symptoms of chronic abdominal and pelvic vein compression are usually gradual in onset and progressive. As the process worsens, you may notice leg swelling, pain, heaviness and aching in the abdomen, pelvis, and legs. With pelvic vein disease your symptoms often worsen with menses and during or after intimacy.
Physical findings with pelvic vein disease include labial varicose veins in women and scrotal veins in men. Varicose veins may also appear in the buttocks and upper thighs along with leg swelling.
The diagnosis of chronic venous compression is based upon symptoms and evidence of venous compression on diagnostic tests. These tests start a venous mapping ultrasound (US) of the thigh and legs. Diagnostic x-ray studies such as an MRI or CT scan, transabdominal US, venogram of the abdominal and pelvic veins, and intravascular ultrasound (IVUS) of the involved veins.
Management recommendations are based on the vein compressed, the degree of compression and your symptoms. We carefully review treatment options with you to help you make an informed healthcare decision. The treatment options include conservative management, minimally invasive endovascular procedures, and traditional surgical options (see below for more treatment details).
The approach to diagnosis and treatment when there are acute symptoms is different. In the setting of an acute DVT of the (iliac and femoral) veins, the onset of pain and swelling in the lower abdomen and legs can be dramatic and sudden. The diagnosis requires an urgent history and physical exam with a combination of duplex US, CT / MRI scan and venogram.
Physical findings include acute worsening swelling and pain. In severe cases the leg can become bluish in color, very tender to touch and the swelling begins to affect the muscles and nerve function.
Management recommendations are based on the physical exam and diagnostic tests. If an emergency US shows DVT from the deep veins of the pelvis into the deep veins of the thigh, immediate actions should be taken. If the venous flow from the leg is blocked, this becomes a limb and life-threatening condition, and immediate anticoagulation and hospitalization for close observation and treatment is needed.




Compression of the left renal vein is often seen in healthy, thin, active females between 20-40 years of age. One theory is that low body fat decreases the cushion separating the renal vein from the artery to the small intestines (superior mesenteric artery) and the aorta resulting in compression of the vein. With compression, scarring of the renal vein occurs, back pressure increases in the left renal vein, and reflux feeds the varicose veins near the kidney, ureter and in the veins draining the left ovary or testicle.
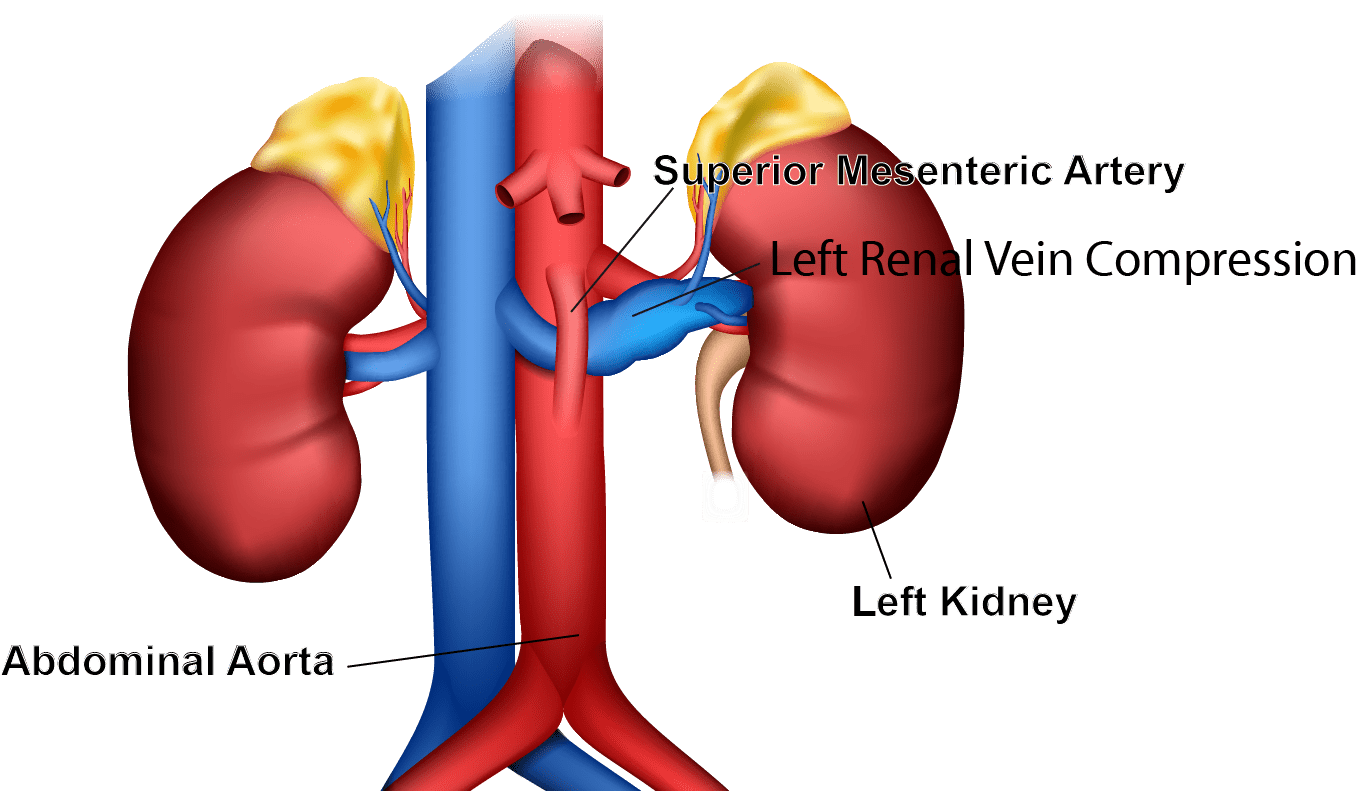
The diagnosis of left renal vein compression (Nutcracker) begins with having a high index of suspicion. Symptoms of left renal vein compression are vague, including pain in the left flank, abdominal pain and fatigue. A history of these symptoms and microscopic blood (hematuria) and protein (proteinuria) in the urine are suggestive of renal vein compression. Additional studies may include abdominal ultrasound, CT, or MRI scans. These studies may help identify good candidates for more further testing and treatment. The definitive diagnosis is made by selective venogram of the renal, ovarian, testicular, and iliac veins with IVUS and pressure gradient measurements in the area of compression.
Overview of Treatment of Left Renal Vein Compression: The VSS approach to treating left renal vein compression is to offer the best treatments based upon symptoms and anatomic findings. Treatments fall into one or a combination of treatment options.
Conservative measures: This condition seems to be more common if you have a low body weight. A modest weight gain in some patients has proven to lessen the compression and symptoms.
Endovascular Procedures: If there is significant symptomatic left renal vein compression dilating the stenotic vein, in some circumstances, placing a stent may be a treatment option. However, this can be a technically challenging procedure with uncertain results.
If you have renal vein compression and ovarian/testicular vein reflux, treating the renal vein stenosis may correct reflux in the left ovarian or testicular veins. On the other hand, treating the ovarian vein reflux while ignoring the renal vein compression make the renal vein stenosis symptoms worse.
Surgical Procedures: In more severe cases, surgical management of the renal vein compression may be indicated. Your VSS team will discuss other treatment options including surgery when appropriate.
The most common anatomic cause of iliac vein compression is when the deep vein that drains the blood from the left leg (left common iliac vein) is compressed between the artery that supplies the blood to the right leg (right common iliac artery) and the spine. This compression over time can have serious consequences.
Other rare causes of iliac vein compression include compression of the right common iliac vein by the right iliac vein. Compression of the left iliac vein by the left common iliac artery, or compression of the left iliac vein by an aneurysmal change of the right common iliac artery.
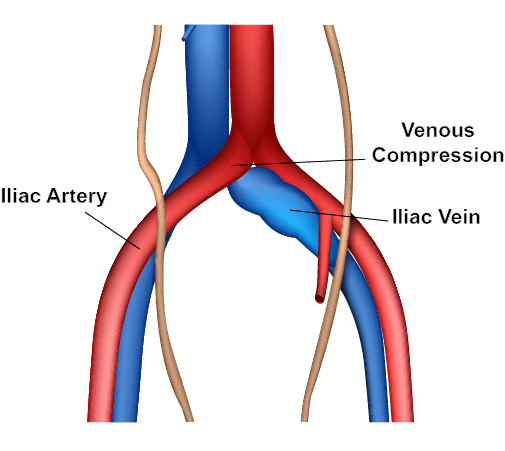
Consequences of iliac vein compression: The chronic and repetitive damage to the iliac vein carries with it an increased risk of DVT in the iliac and deep veins on the thigh and leg. Varicose veins which develop secondary to iliac vein disease lead to symptoms of chronic venous insufficiency such as heavy achy legs, swelling, pain, tenderness, skin changes and venous ulcers. In some patient’s, iliac vein reflux may be associated with pelvic varicose veins with or without ovarian vein reflux. In these patients it can contribute to pelvic congestion symptoms including pelvic pain with menses and during or after intercourse.
The diagnosis of left iliac vein compression begins with having a high index of suspicion. You may have no, or vague symptoms, of left iliac vein compression including heaviness in the thigh or leg with aching pain and swelling. The most likely reason you might see a vein specialist for an evaluation would be symptomatic varicose veins or leg swelling and pain.
Chronic symptoms and physical findings of iliac vein compression: Left lower extremity pain aggravated with standing or sitting is a common symptom. This swelling can be accompanied by physical findings of varicose veins, swelling, skin changes and leg ulcers in the chronic venous stasis phase. Large varicose veins may be seen on physical exam or ultrasound across the lower abdomen if there is already iliac vein obstruction.
Acute symptoms and physical findings of an iliac vein DVT: The first symptom of an iliac vein compression with acute DVT and or PE may be acute pain in the leg or chest pain. Physical symptoms include sudden swelling of the thigh and leg. As the process worsens, the leg can take on a bluish hue, become tender to touch, and show signs of muscle weakness and nerve damage. This is a medical emergency requiring immediate care to avoid loss of limb or life. If you experience these symptoms call 911 and get evaluated. Remember to ask the doctor ‘how do you know I don’t have a blood clot?
Treatment Overview for Iliac Vein Compression: There is debate among vein specialists on who should have their iliac vein compression treated and when. Your treatment decision depends upon multiple factors with the intent of improving your quality of life and health. At VSS we seek to provide the best vein care with WOW service while avoiding unnecessary procedures.
Treatment criteria: Significant compression of the left iliac vein is >50% narrowing of the iliac vein lumen based on IVUS studies. However, clinical studies have shown that 25% of patients with significant compression of their iliac vein may be asymptomatic. Therefore, clinically significance is based upon the symptoms, % of compression of the iliac vein on IVUS, and changes in venous flow or venous pressure. This evidence includes vein flow reversal, the presence of collateral veins and varicose veins. A history of acute or chronic DVT in the iliac vein or scarring of the vein is a significant finding that may be used to over-ride other criteria for treatment.

It’s just 3 easy steps…



Conservative measures: If you do not have an acute or chronic iliac vein DVT at the time of your diagnosis, conservative treatment measures including compression, elevation, exercise, and healthy weight management are recommended. These conservative care measures may alleviate some of the chronic symptoms. If you have chronic scarring in the iliac vein, anticoagulation may be added to the treatment plan to lower the risks of a recurrent DVT. In these situations, monitoring for progression may be considered.
Elective Endovascular Procedures: If you have clinically significant left iliac vein compression with symptoms, dilating the stenotic vein with or without stent placement may be considered to relieve symptoms and lower the risks of a serious consequences of an acute iliac vein DVT.
Venogram and endo-venous IVUS studies are performed on an out-patient basis in our vascular therapy lab, often with the understanding that treatment may be offered at the same setting or later. If you have vein dilation and stenting, periodic follow-up ultrasound studies and a period of anticoagulation or antiplatelet therapy may be needed. Treating the iliac vein stenosis may correct some pelvic vein disease symptoms.
If you have severe venous outflow obstruction from a proximal DVT in the iliac and common femoral veins Thrombolytic Therapy is indicated. This minimally invasive treatment involves a clot-dissolving medication delivered through a catheter into the clot. Dissolution occurs within a matter of hours or days. After clot removal, the iliac vein can be evaluated with IVUS to identify significant narrowing of the iliac vein.
Angioplasty/stenting is a minimally invasive treatment to widen the narrowed area of the iliac vein using either a balloon or a stent to open the vein for free blood flow. Stenting prevents the iliac artery from compressing the iliac vein in the future. If symptoms recur following stent placement, stent re-stenosis and thrombosis should be suspected, investigated, and treated.
Vena cava filters are for patients who cannot take blood thinners or those who have recurrent Pulmonary Emboli (PE) while being treated for a DVT. It involves inserting the filter into the vena cava (the body’s largest vein) to prevent clot migration. It does not stop clots from forming, but it prevents them from reaching the lungs.
Surgical Procedures for iliac vein compression: In more severe or unresponsive cases, traditional surgical management of the iliac vein compression may be needed to address the problem.
Iliac artery repositioning shifts the relationship behind the iliac artery and vein, so it no longer compresses it. An alternative to repositioning surgery is creating a tissue sling to act as a cushion between the two blood vessels.
In some cases, open surgical thrombectomy may be needed for large clots or those causing severe tissue damage.
Your VSS team will discuss other treatment options including surgery when appropriate.
Receive a FREE resource via email about non-surgical treatments and how we can help.

Since 1997, Vein Specialists of the South has helped thousands of patients like you with varicose veins, spider veins, and leg swelling. Dr. Kenneth Harper is a leader in vein health is a Diplomat of the American Board of Surgery and the American Vein and Lymphatic Medicine. Terri Harper, MSN, FNP-C, is a renowned educator in the field of cosmetic sclerotherapy. Our dedicated nurse injectors have been trained by the best.
At Vein Specialists of the South, we have a passion for veins – big and small. We’ve helped over 30,000 people get Better Veins for Life®. Call today to schedule an appointment with the VSS team, where ‘Veins Aren’t Just One Thing We Do, They Are the Only Thing We Do.®’
Meet with your dedicated vein care specialists to get started on your personalized comprehensive treatment plan.

*Individual Results May Vary

556 3rd Street, Suite A
Macon, Georgia 31201
4851 Bill Gardner Pkwy,
Locust Grove, GA 30248
151 South Houston Lake Rd
Warner Robins, Georgia 31088
© Copyright 2024 Vein specialists of the south | Terms of Use | Website Privacy Policy | Medical Privacy Policy
Complete the information below to receive a Receive a FREE resource about non-surgical treatments and how we can help.
Ready to learn how we can help you enjoy Better Veins for Life®?
Complete the information below to receive a FREE resource about varicose veins.